Let’s be honest: most of us grew up thinking that our period was just a few days of bleeding, cramps, and chocolate cravings. But what if I told you that this is only a small chapter in a much bigger, more powerful story happening inside our bodies each month?
School barely scratched the surface. We weren’t taught that two overlapping cycles, the ovarian cycle and uterine cycle, govern everything from our mood and energy levels to our skin, digestion, and how we connect with others. Yet, most women go through decades of these cycles without truly understanding what’s going on inside them, when,how or why. That’s not just a knowledge gap, it‘s a disconnection from our very nature.
When we really understand our cycle, we unlock one of the most powerful tools for boosting our health, enhancing our sex life, improving fertility, lifting our mood, optimizing our workouts, and even boosting productivity.

Table Of Contents
Introduction
As women, we don’t just experience a calendar month, we go through a physiological month – an internal rhythm that starts on the first day of bleeding and continues until the next period. Unlike the standard calendar, which is the same across the board, our cycles are unique.
Learning to track ours helps us perform at our best. After all, Our menstrual cycle influences nearly every aspect of our lives – our relationships, libido, energy and productivity.
Typically, the cycle lasts around 28 days, but it can range from 21 to 35 days. from your first period- menarche- to menopause, your cycle may change, especially if you have conditions like pcos.
To figure out your cycle length, start counting from the first day of heavy bleeding, what we call “day 1” up to the day your next period begins. If you notice light spotting before your heavy bleeding at the beginning of your period, that doesn’t count as part of this cycle; it‘s just the tail end of your last one.
What makes this entire process so confusing is the complex hormonal interaction between your brain, ovaries and uterus. It‘s all about two interconnected cycles working simultaneously:
- The Ovarian cycle: It includes all changes during menstrual cycle in the ovaries.
- The Uterine cycle: it includes all changes during menstrual cycle in the uterus.
Although we often talk about these cycles separately, they’re actually tightly linked, influencing each other throughout the month. Both have distinct phases, with many changes occurring inside your ovaries and uterus during each one.
The ovarian cycle has three main phases: 1. follicular, 2. ovulation, and 3. luteal. Meanwhile, the uterine cycle includes four phases : menstruation, proliferative phase, ovulation and secretory phase.
The Ovarian Cycle
Phase 1: The Follicular Phase
This phase kicks off at the start of your period, as your undeveloped follicles begin to mature, reaching readiness for ovulation and continuing until your ovulation. It lasts about 14 days on average but can be shorter or longer- depending on how long it takes for your follicles to mature- anywhere from 7 to 21 days.
Follicles are fluid filled sacs in your ovaries that house immature eggs. Every woman is born with millions of these, but by puberty, their number drops around 300,000-400,000. Each month, during the follicular phase, only one follicles fully matures and releases an egg.
This process will be regulated by both of your ovaries and brain, your hypothalamus in the brain acts as the control center for this process. At the start of follicular phase your hypothalamus receives feedback from your ovaries that is the time of follicle maturation. The hypothalamus then releases hormones that prompt the pituitary gland – located on the base of your brain- to secret Follicle stimulating Hormones ( FSH).
FSH stimulates your ovaries to develop follicles; among these, one is healthier and becomes mature more quickly- that is known as your dominant follicle (Graafian follicle) which is the one that releases mature egg.
As these follicles develop and become bigger, they release estrogen hormone, specially your dominant follicle releases lots of it. Rising estrogen levels triggers the pituitary gland to slow down the FSH production, which leads to other less- developed follicles wither away and reabsorbed by your ovaries.
Toward the end of the follicular phase, your rising estrogen triggers the pituitary gland to release Luteinizing hormone (LH). LH stimulates follicular growth but what makes this hormone really important is the phenomenon known as „ LH Surge“ which occurs around the 36 to 40 hours before ovulation. This is the time in your cycle that you are most likely to get pregnant.
During this phase, many women notice improvements in skin health and overall well- being. that‘s because higher estrogen boosts collagen, hyaluronic acid, and elastin, making your skin more radiant and your hair shinier.
Plus, estrogen boosts your confidence and motivation, making it an ideal period to tackle new projects, setting a goal, and focusing on self care. Also in the follicular phase your energy level, libido and sexual desire increase, thanks to high levels of estrogen.
Although this phase is generally beneficial, for some women it could cause irritability and mood swings due to fluctuating hormone level.
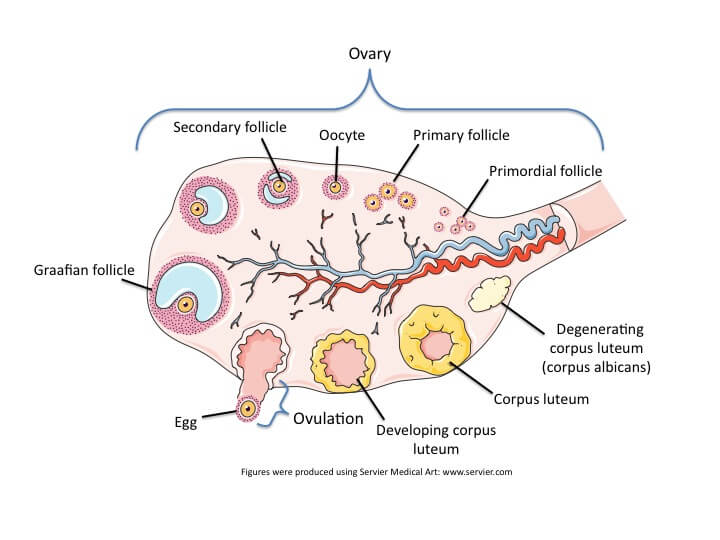
Figure 1.upper
Phase 2: Ovulation
The LH surge causes your dominant follicle to swell, rupture and release an egg into your fallopian tube, this process called ovulation, which it take only a few minutes, although final swelling stages could take a few hours but the rapture takes only few minutes, some women sometimes feel mild pain on both sides of lower pelvis, where the ovaries located. (Figure 1.)
Right after ovulation the estrogen level drops drastically. This phase normally occurs around day 14 of your cycle, but if you have a longer follicular phase, then it could take longer.
Interestingly, this is also when your Libido peaks, thanks to high levels of estrogen and testosterone which heightened sexual desire, attractiveness and arousal. Plus they improve mood, and enhance cognitive flexibility ,which can contribute to greater creativity and originality in this time.
phase 3: luteal phase
12Post ovulation, the empty follicle structure (think of it as an empty sac, with thick wall) transforms into a temporary gland called corpus luteum ( yellow body), which secretes Progesterone and a little estrogen. (Figure 1.)
Progesterone is one of the most Important Hormones in your body, it prepares the uterus for pregnancy by thickening the lining and nourishing a fertilized egg if conception occurs. It also has anti-inflammatory effects.
Unlike the follicular phase, this phase has a fixed number of days, about 14-16 days, from ovulation until your next period.
The drastic hormone fluctuations here are mainly responsible for mood swings, headaches and many PMS ( Premenstrual syndrome) symptoms.
If fertilisation happens, the corpus luteum persists for about three months, supporting early pregnancy, until full development of the placenta, which after that it takes over the job of progesterone production. If not, it degenerates into corpus albicans (or white body), which loses its ability to secrete hormones.
This drop of hormone levels, is a signal to uterus to shade. It marks the end of this menstrual cycle, and beginning of a new ovulatory cycle.
During this time, cravings and metabolic rate tend to increase, leading to higher calorie needs, to maintain stable blood sugar. Libido generally drops because high progesterone level acts as a negative predictor of sexual desire, but it can vary from woman to woman, also some women experience mood swing.
The Uterine cycle:
This cycle mirrors and runs parallel to the ovarian cycle, involving the changes within your uterus.
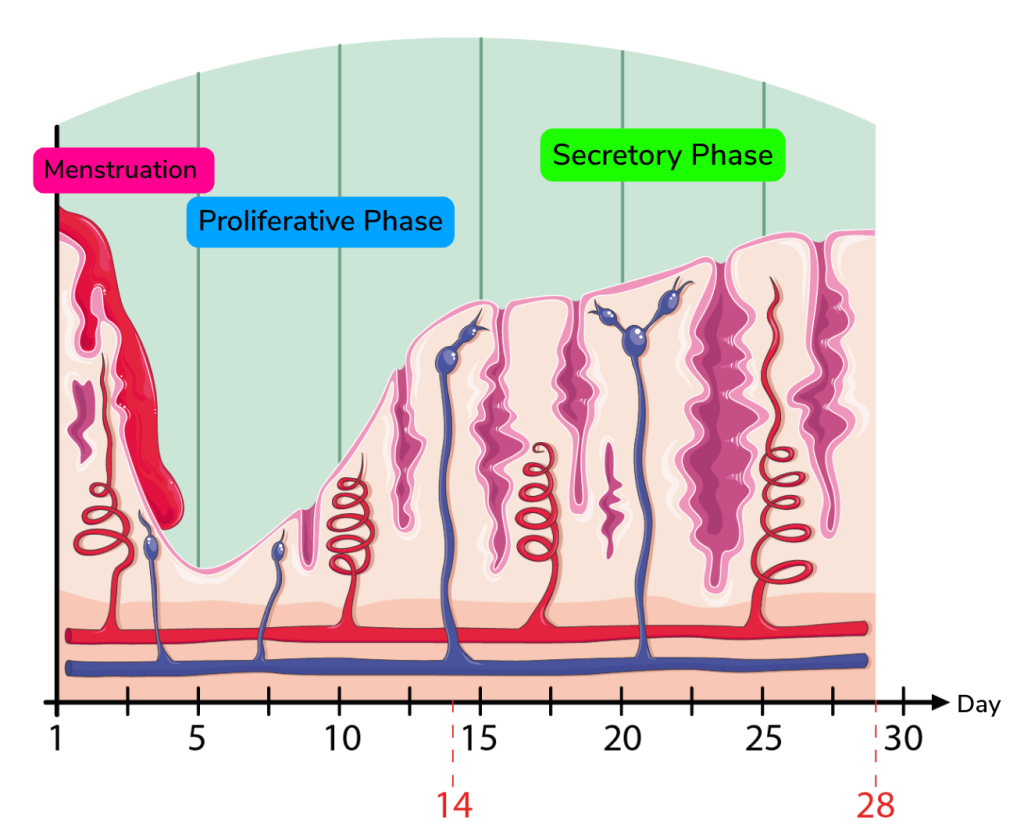
Figure 2.
Phase 1: Menstruation ( the period):
This is the most obvious phase, the start of your cycle marked by bleeding as the uterine lining (endometrium) sheds due to falling levels of progesterone and estrogen.
Despite general believes your menstrual fluid is not all blood, it contains some blood, cervical mucus, vaginal secretions, and some uterine lining ( endometrial tissue).
what is Endometrial lining?
Think of your Uterus as a cup with three layers: the innermost layer rich with blood vessels this area called Endometrium, the middle muscular layer, responsible for contraction of the uterus during the labor, called Myometrium, and outer Perimetrium, which protects the entire structures.
During menstruation only one third of the upper part of your endometrium sheds, two thirds of it remains as the base for generating your uterus lining for your next cycle.
Your menstruation phase typically last about 5-7 days, and in average you will loss 50 ml of menstrual fluid, but this could change between 25 ml ( scanty flow ) to 80 ml ( heavy flow) (Figure 2.)
phase 2: The proliferative phase
Starting after your period ends, as your follicles mature and produce estrogen, your endometrium which already lost its upper layer begins to rebuild and thicken to preparing for a possible pregnancy.
phase 3: Ovulation
This is a transition phase where the mature egg is released following the LH surge, marking the shift from the proliferative phase to secretory phase.
phase 4: the Secretory phase
Following ovulation, progesterone from corpus luteum causes the endometrial lining, which already thickened during the last phase, to become more glandular and secretory and nutrient- rich, creating an environment ideal for implantation.
If fertilization does not occur, the corpus luteum degenerates, the progesterone and estrogen level drops, causing the lining to break down and shed, starting new cycle.
conclusion:
Your cycle is much more than a lengthy gap between your bleeding, it is an intricate symphony conducted by your brain, ovaries and uterus.
Next time you notice some changes in your hair, skin, mood or energy, instead of judging yourself or beating yourself up, take a moment to identify where you are in your cycle; are you in your follicular phase or luteal phase? Recognizing which hormones are dominant can help you better understand yourself and find tailored solutions, especially if you have PCOS.
By understanding your menstrual cycle and ovulation you can better manage your symptoms.

